Specific Applications of Dental CAD/CAM Digital Manufacturing Technology in Dentistry
2024-10-19
2026-02-01
In modern dental CAD/CAM systems, zirconia blocks have become a cornerstone for fabricating durable and aesthetically pleasing restorations. Zirconia, a ceramic material known for its biocompatibility and mechanical properties, is available in various formulations. Two primary categories dominate: high translucency zirconia (often 4Y or 5Y yttria-stabilized) and standard zirconia (typically 3Y yttria-stabilized). High translucency zirconia prioritizes light transmission for natural-looking results, while standard zirconia emphasizes superior strength for functional demands. This article compares their properties and provides practical adaptation recommendations for different dental restoration scenarios, helping clinicians select the optimal material based on clinical needs.
Zirconia blocks are milled using CAD/CAM technology, allowing precise customization for crowns, bridges, veneers, and implants. The choice between high translucency and standard variants depends on factors like location (anterior vs. posterior), patient habits (e.g., bruxism), and aesthetic requirements. Data from studies indicate that while high translucency zirconia offers translucency parameters (TP) ranging from 9 to 29 at 1 mm thickness, standard zirconia typically shows lower TP values of 4 to 10, making it more opaque but stronger. Flexural strength for standard zirconia often exceeds 900-1200 MPa, compared to 500-800 MPa for high translucency types. Understanding these differences ensures restorations that balance aesthetics and longevity.

Translucency is measured by the translucency parameter (TP), which quantifies light transmission through the material. Higher TP values indicate better light diffusion, mimicking natural tooth enamel (TP ≈18.7) and dentin (TP ≈16.4). High translucency zirconia achieves TP values of 9.37-29.7 at 1 mm, making it suitable for scenarios requiring lifelike appearance. This is due to increased cubic phase content (up to 50% in 5Y formulations), which enhances light scattering without compromising basic integrity.
In contrast, standard zirconia has a predominantly tetragonal phase, resulting in TP values of 4.43-10 at similar thicknesses. It appears more opaque, which can be advantageous for masking discolored abutments but limits its use in visible areas. Studies show that thinner restorations (0.5 mm) of high translucency zirconia exhibit higher TP (e.g., 11.51 using CIE-Lab), decreasing to 6.54 at 1.5 mm, highlighting thickness's impact on aesthetics.
Aesthetically, high translucency zirconia rivals lithium disilicate glass-ceramics, with comparable TP values, but offers better fracture resistance. Standard zirconia, while less translucent, can be layered with porcelain for improved visuals, though this may introduce chipping risks.
Flexural strength is critical for withstanding occlusal forces. Standard zirconia boasts 900-1500 MPa, making it ideal for high-stress applications. Its transformational toughening—where tetragonal grains convert to monoclinic under stress—prevents crack propagation. High translucency zirconia, with more cubic content, has lower strength (500-900 MPa), but still surpasses porcelain-fused-to-metal (PFM) restorations (typically 100-500 MPa).
Durability tests reveal an inverse relationship: higher translucency correlates with reduced strength (correlation coefficient r ≈ -0.77). Standard zirconia resists wear better in bruxism cases, with minimal degradation after thermocycling. Both types are biocompatible, with low plaque accumulation and excellent marginal fit via CAD/CAM.

Fracture toughness for standard zirconia is higher (5-10 MPa·m^(1/2)) than high translucency (3-5 MPa·m^(1/2)). Wear on opposing enamel is comparable for both, but polished surfaces minimize abrasion. Aging resistance is strong in both, though high translucency may show slight TP reduction post-fatigue.
For anterior crowns, aesthetics are paramount. High translucency zirconia is recommended due to its enamel-like light transmission, achieving seamless integration with adjacent teeth. With TP values approaching 18-20, it suits minimal preparations (0.7-1.25 mm reduction) and cases with moderate discoloration. Monolithic designs reduce chipping risks, and multilayer blocks enhance shade gradients.
Standard zirconia is less ideal here unless layered with porcelain, as its opacity can create a "gray line" at margins. Use it only if strength overrides aesthetics, e.g., in parafunctional patients with anterior wear.
Posterior crowns demand durability under heavy loads. Standard zirconia excels with flexural strength >1000 MPa, suitable for molars and premolars in bruxism or high-occlusion cases. Minimal reduction (0.5-1.0 mm) preserves tooth structure, and its opacity masks dark stumps.
High translucency zirconia can be used for visible premolars if aesthetics matter, but its lower strength (600-800 MPa) limits it to low-stress scenarios. Avoid in severe bruxers.
For bridges (up to 3-4 units), standard zirconia is preferred for its high strength, supporting spans without fracture. It withstands connector stresses (minimum 9-12 mm² cross-section) in posterior regions. Clinical data show survival rates >95% over 5-6 years.
High translucency zirconia suits anterior bridges (up to 3 units) for better translucency, but requires thicker connectors (12-16 mm²) due to reduced toughness. For longer spans, combine with standard for frameworks.
Veneers benefit from high translucency zirconia's thin fabrication (0.3-0.5 mm), providing natural opacity gradients. It's ideal for anterior esthetics, with bond strengths comparable to glass-ceramics after priming.
Standard zirconia is rarely used for veneers due to opacity but works for posterior inlays/onlays needing strength. Its wear resistance protects occlusal surfaces.
In implant prosthetics, standard zirconia is recommended for abutments and full-arch hybrids, offering strength (1000+ MPa) and biocompatibility. It reduces mucosal discoloration compared to metals.
High translucency suits anterior implant crowns for aesthetics, but ensure sufficient thickness to avoid fractures.
For complex cases, hybrid approaches work best: high translucency for anterior zones and standard for posterior. This balances load distribution and visuals, with CAD/CAM ensuring precise occlusion.

Patient-specific factors influence choices: bruxism favors standard zirconia, while high-value smiles prefer high translucency. Thickness affects both—reduce for high translucency to boost TP, but maintain minimums (0.5 mm occlusal) for strength.
Fabrication tips: Use digital workflows for accuracy; sinter at recommended temperatures to preserve properties. Cementation with resin cements enhances bonding, especially for high translucency. Long-term data show both types have high survival (90-98% at 5 years), but monitor for low-temperature degradation in humid environments.
High translucency zirconia excels in aesthetic-driven scenarios like anterior crowns and veneers, offering TP values close to natural teeth with adequate strength. Standard zirconia dominates functional applications such as posterior bridges and bruxism cases, with unmatched flexural strength. In dental CAD/CAM systems, selecting the right block optimizes outcomes—balancing translucency, durability, and patient needs. Clinicians should evaluate each case holistically, leveraging these recommendations for superior restorations. Future advancements may further blur lines between variants, enhancing versatility in aesthetic dentistry.

Dry & wet milling for zirconia, PMMA, wax with auto tool changer.
learn more
High-precision 3D scanning, AI calibration, full-arch accuracy.
learn more
40-min full sintering with 57% incisal translucency and 1050 MPa strength.
learn more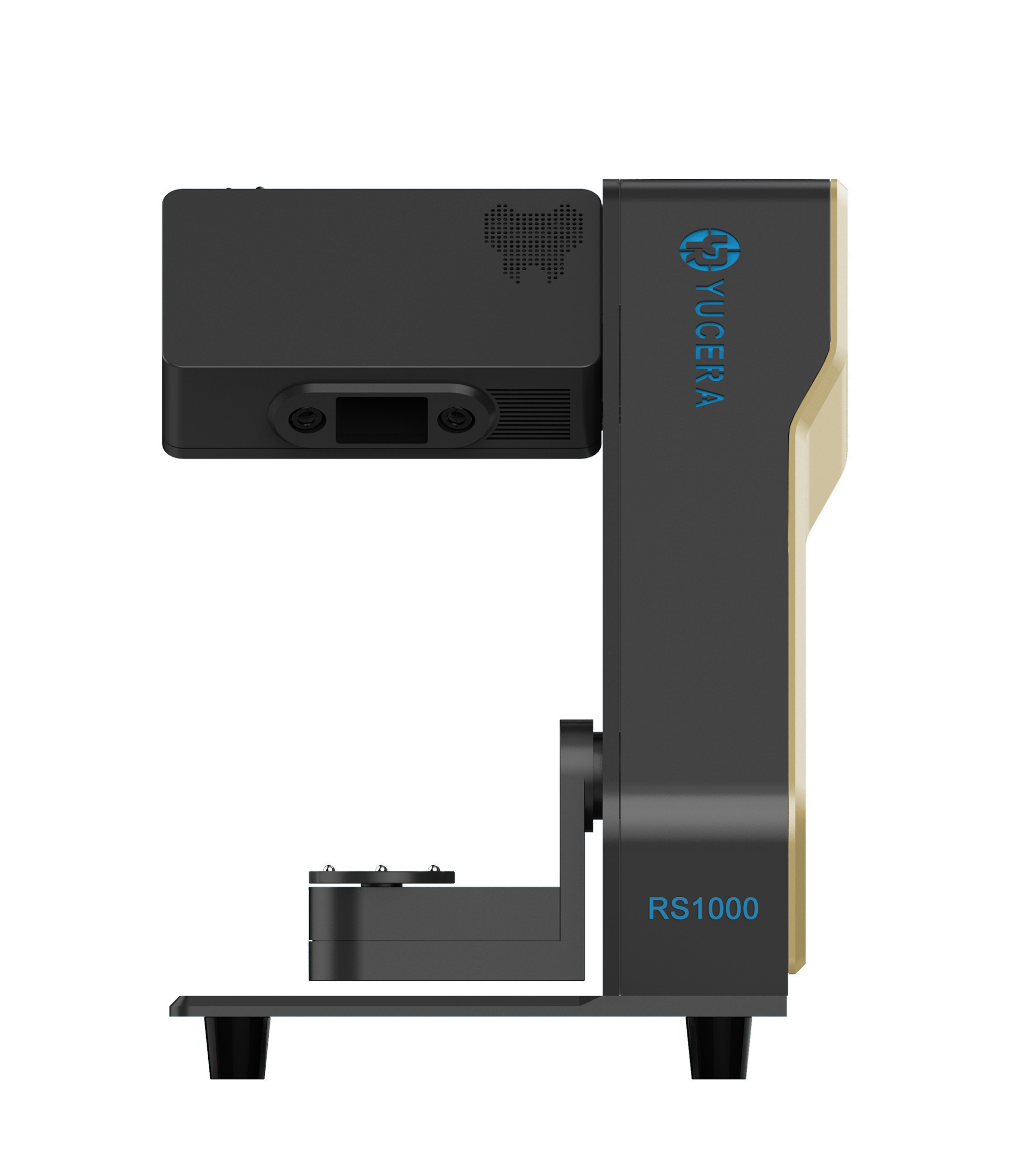

40-min cycle for 60 crowns, dual-layer crucible and 200°C/min heating.
learn more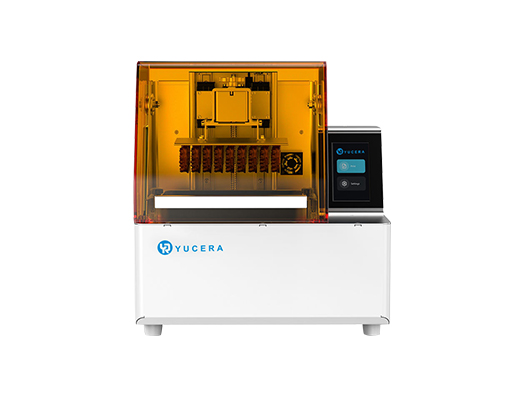
High-speed LCD printer for guides, temporaries, models with 8K resolution.
learn more