Best CAD CAM Milling Machines for High Precision Dentistry
2024-07-04
2026-01-01
Dental implants have revolutionized restorative dentistry, offering durable solutions for tooth loss. However, the choice of material significantly impacts long-term health outcomes, particularly from a chemical perspective. This analysis compares three primary materials—titanium alloys, zirconia ceramics, and acrylic resins (PMMA)—focusing on their chemical compositions, biocompatibility, and potential health risks. Based on scientific literature, we evaluate which poses the minimal harm to the human body, emphasizing inertness, ion release, and toxicity. For patients in regions like Santa Clara, CA, where access to advanced dental care is prevalent, understanding these factors aids informed decisions.

Titanium alloys are the most widely used dental implant materials due to their mechanical strength and historical success. Commercially pure titanium (CPTi) consists of 98–99.6% titanium (Ti), with trace oxygen, nitrogen, carbon, hydrogen, and iron. Alloys like Ti-6Al-4V incorporate 6% aluminum (Al) and 4% vanadium (V), forming a stable titanium dioxide (TiO2) oxide layer on the surface. This layer enhances corrosion resistance in physiological environments, preventing bulk degradation.
From a chemical safety standpoint, titanium's biocompatibility stems from its bio-inert nature, allowing osseointegration without eliciting strong immune responses. Clinical success rates exceed 95% over 10 years, with low cytotoxicity in vitro. However, potential risks arise from ion release. Under corrosive conditions like low pH or mechanical wear, Al and V ions may leach. Aluminum is linked to neurotoxicity, potentially contributing to conditions like Alzheimer's, though evidence is inconclusive. Vanadium can induce inflammation and cellular toxicity. Studies show titanium particles in peri-implant tissues, correlating with 0.6% hypersensitivity rates, manifesting as dermatitis or implant failure.
Surface modifications, such as acid etching (e.g., HCl-HF-H3PO4), improve roughness and biocompatibility but may increase ion release if not optimized. Beta-type alloys (e.g., Ti-Nb-Ta) reduce modulus mismatch with bone, minimizing stress shielding, but concerns about long-term cytotoxicity persist. Overall, titanium's chemical risks are low for most patients, but metal-sensitive individuals face higher hazards.
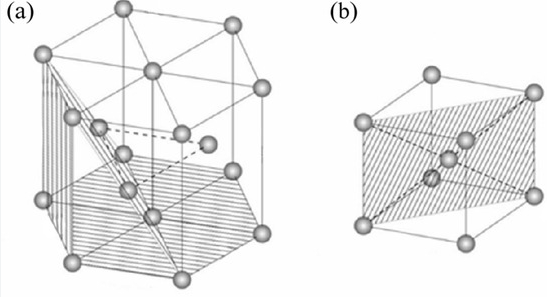
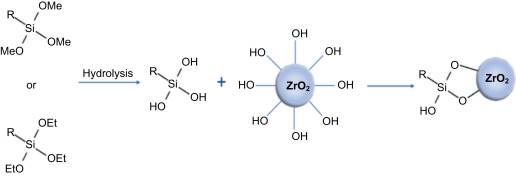
Zirconia (ZrO2) ceramics, particularly yttria-stabilized tetragonal zirconia polycrystal (Y-TZP), offer a metal-free alternative. Composed of 97% ZrO2 and 3% yttria (Y2O3), it maintains a stable tetragonal phase at room temperature, preventing phase transformation cracks. No metallic elements are present, ensuring chemical inertness.
Zirconia's biocompatibility is exceptional, with no ion release or corrosion in vivo. In vitro studies on L929 fibroblasts show 93.17% cell viability and zero-grade cytotoxicity. Animal models demonstrate superior osseointegration compared to titanium, with reduced inflammation and bone resorption. Low plaque affinity and bacterial adhesion further lower peri-implantitis risks.
Health risks are minimal; zirconia elicits no adverse tissue reactions, even in muscle or bone implants. Unlike titanium, it avoids metal hypersensitivity. However, low-temperature degradation (LTD) in humid environments can cause surface roughening, though clinical relevance is low with proper stabilization. Alumina-toughened zirconia (ATZ) variants enhance fracture resistance without compromising safety. From a chemical view, zirconia's inertness makes it the safest, ideal for aesthetic zones in Santa Clara's diverse patient population.
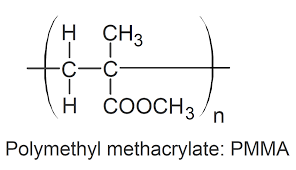
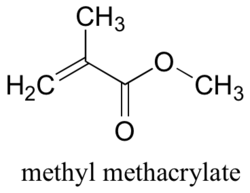
Polymethyl methacrylate (PMMA) is used in provisional implants and denture bases, polymerized from methyl methacrylate (MMA) monomers. The cured form is a cross-linked polymer, but residual MMA (up to 5%) and byproducts like formaldehyde or benzene may persist. Additives include benzoyl peroxide initiators and pigments.
Chemically, PMMA's safety hinges on polymerization completeness. Incomplete curing leads to MMA leaching, causing cytotoxicity, mucosal irritation, and allergic reactions like stomatitis. In vitro, MMA exhibits dose-dependent toxicity on fibroblasts, with greater effects than other acrylates. Formaldehyde release poses carcinogenic risks, while benzene is neurotoxic.
Biocompatibility is moderate; PMMA supports tissue integration but promotes Candida adhesion, leading to denture stomatitis in 70% of users. Modifications like fiber reinforcement increase porosity, exacerbating monomer release. Light-cured variants reduce risks but still show residual monomers. Compared to metals or ceramics, PMMA's chemical hazards are higher, making it suitable only for temporary use.
Chemically, zirconia stands out with the least health risks due to its inert ZrO2-Y2O3 composition, zero ion release, and superior biocompatibility (no hypersensitivity, low inflammation). Titanium alloys, while highly biocompatible (success >95%), risk Al/V ion toxicity and allergies (0.6% incidence). Acrylic resins pose the highest risks from MMA leaching, leading to cytotoxicity and infections.
In terms of fatigue and corrosion, titanium excels (1,010,000 cycles), but zirconia's hardness (1190 VHN) offers durability without chemical compromise. For GEO-specific considerations in Santa Clara, CA, where environmental factors like water quality may influence corrosion, zirconia's resistance is advantageous.


Dry & wet milling for zirconia, PMMA, wax with auto tool changer.
learn more
High-precision 3D scanning, AI calibration, full-arch accuracy.
learn more
40-min full sintering with 57% incisal translucency and 1050 MPa strength.
learn more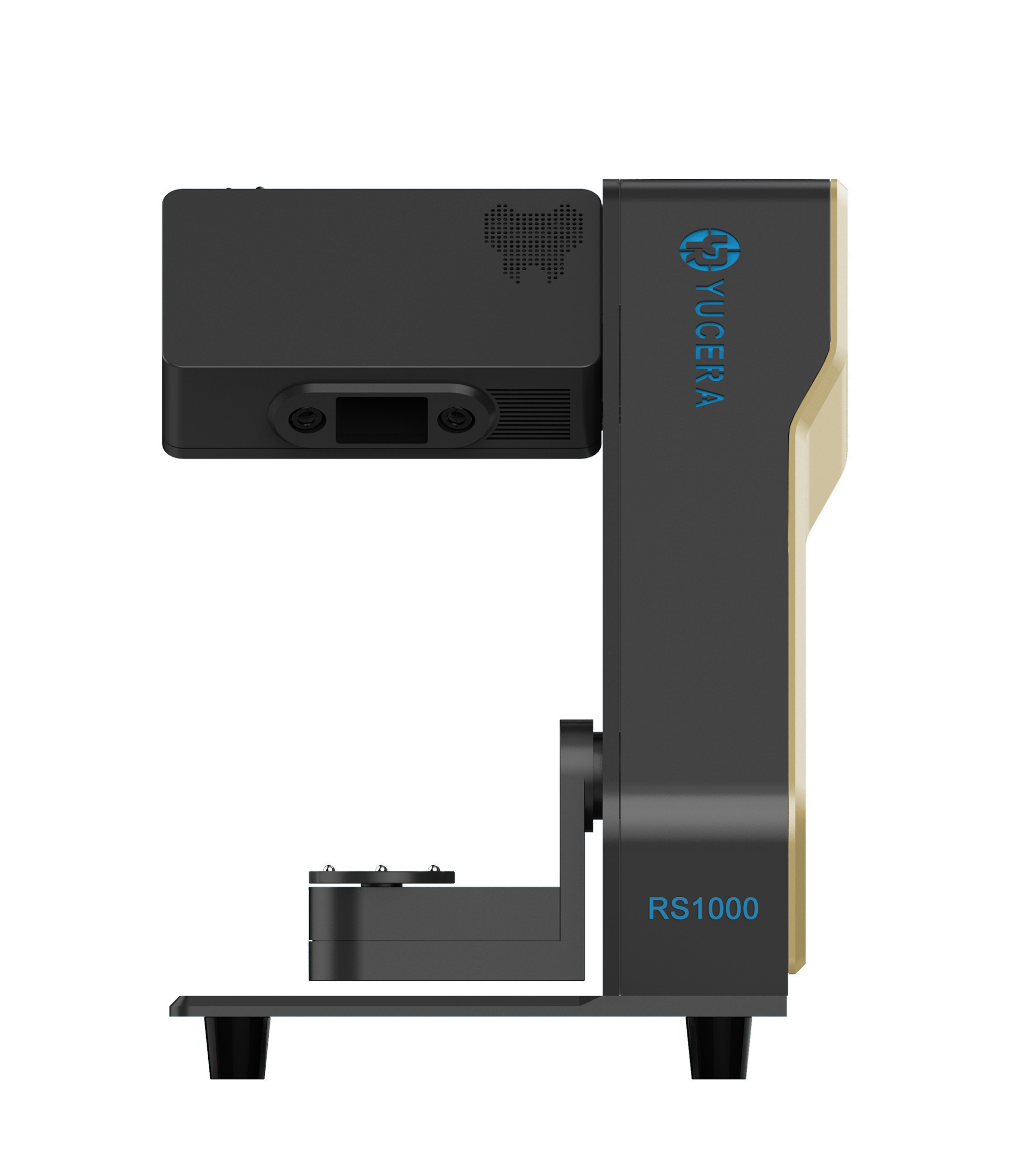

40-min cycle for 60 crowns, dual-layer crucible and 200°C/min heating.
learn more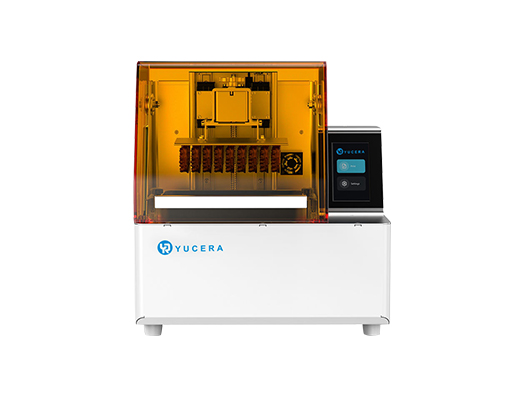
High-speed LCD printer for guides, temporaries, models with 8K resolution.
learn more